Understanding Type 1 Diabetes: A Comprehensive Guide

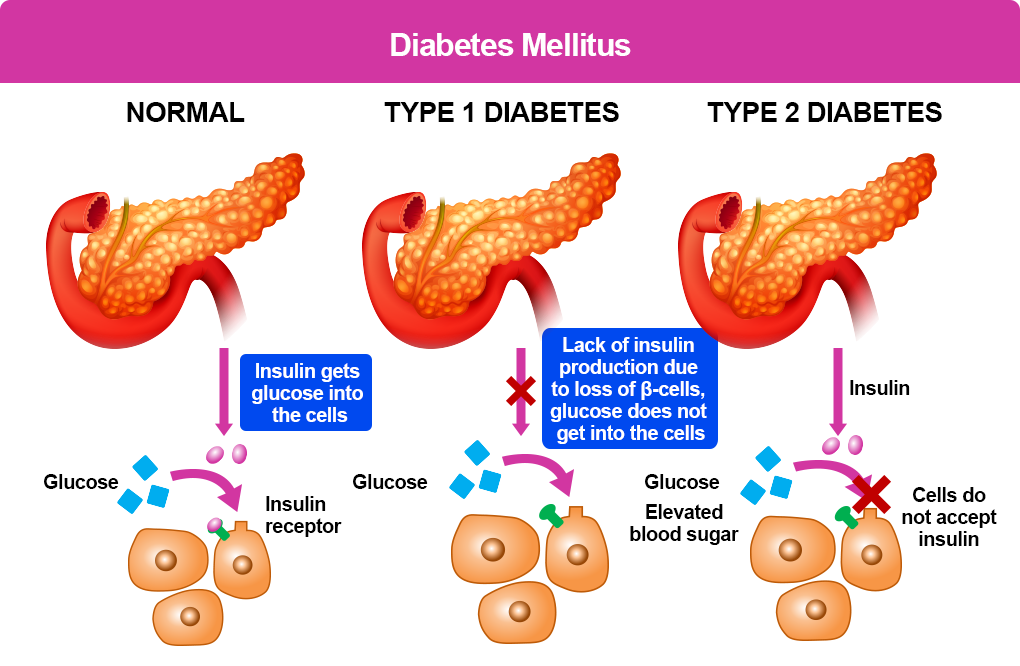
Type 1 diabetes, once known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition that affects how your body regulates blood sugar. Unlike type 2 diabetes, which is often associated with lifestyle factors, type 1 diabetes is an autoimmune disease. This means that your body’s immune system mistakenly attacks and destroys the insulin-producing cells in your pancreas.
What is Insulin and Why is it Important?
Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels. It acts like a key, unlocking your cells to allow glucose (sugar) to enter and be used for energy. When you eat carbohydrates, your body breaks them down into glucose, which is then released into your bloodstream. Insulin helps transport this glucose into your cells, preventing it from building up to dangerous levels.
The Role of the Immune System in Type 1 Diabetes
In people with type 1 diabetes, the immune system mistakenly identifies the insulin-producing cells in the pancreas as foreign invaders. It launches an attack, destroying these cells and leaving the body unable to produce insulin. This leads to a chronic shortage of insulin, causing blood sugar levels to rise.
Symptoms of Type 1 Diabetes
The symptoms of type 1 diabetes can develop rapidly and often include:
- Frequent urination: As your blood sugar levels rise, your kidneys work overtime to filter excess glucose, leading to increased urination.
- Excessive thirst: Dehydration is a common symptom of high blood sugar. Your body may signal thirst as it tries to compensate for fluid loss.
- Extreme hunger: Despite eating, you may feel constantly hungry. This is because your body can’t use the glucose for energy, leading to a persistent feeling of hunger.
- Unexplained weight loss: When your body can’t use glucose for energy, it starts breaking down muscle and fat for fuel, leading to weight loss.
- Fatigue: Low energy levels and fatigue can occur as your body struggles to function without adequate glucose.
- Blurred vision: High blood sugar can affect the lens of your eye, causing temporary vision problems.
- Slow-healing sores: High blood sugar can impair blood flow, making it harder for wounds to heal.
- Frequent infections: High blood sugar can weaken your immune system, making you more susceptible to infections.
If you experience any of these symptoms, it’s important to see a doctor for diagnosis and treatment.
Diagnosis of Type 1 Diabetes
Diagnosing type 1 diabetes involves a combination of medical history, physical examination, and laboratory tests. Your doctor may perform the following tests:
- Blood glucose test: This test measures the amount of glucose in your blood.
- Hemoglobin A1c test: This test measures your average blood sugar level over the past two to three months.
- Autoantibody tests: These tests can identify specific antibodies that target the insulin-producing cells in your pancreas.
- Urine test: A urine test can detect the presence of glucose and ketones, which are byproducts of fat breakdown.
Treatment of Type 1 Diabetes
Currently, there is no cure for type 1 diabetes. However, it can be effectively managed with insulin therapy, regular blood sugar monitoring, and a healthy lifestyle.
Insulin Therapy:
- Insulin injections: Insulin is typically administered through daily injections or a continuous subcutaneous insulin pump.
- Insulin pens: These are pre-filled devices that make insulin injections more convenient.
- Insulin pumps: These devices deliver a continuous flow of insulin throughout the day, mimicking the body’s natural insulin production.
Blood Sugar Monitoring:
- Blood glucose meters: These devices measure the amount of glucose in a small blood sample taken from your fingertip.
- Continuous glucose monitors (CGMs): These devices use a sensor inserted under your skin to continuously monitor your blood sugar levels and transmit the data to a receiver.
Healthy Lifestyle:
- Diet: A balanced diet low in carbohydrates and high in fiber can help regulate blood sugar levels.
- Exercise: Regular physical activity can improve insulin sensitivity and help control blood sugar.
- Weight management: Maintaining a healthy weight can help improve insulin sensitivity.
- Stress management: Stress can affect blood sugar levels, so finding healthy ways to manage stress is important.
Complications of Type 1 Diabetes
If type 1 diabetes is not well-managed, it can lead to serious complications, including:
- Diabetic ketoacidosis (DKA): This is a life-threatening condition that occurs when your body produces high levels of ketones, a byproduct of fat breakdown. Symptoms include nausea, vomiting, abdominal pain, rapid breathing, and confusion.
- Hypoglycemia: This occurs when your blood sugar levels drop too low. Symptoms include sweating, shaking, dizziness, and confusion.
- Heart disease: High blood sugar can damage blood vessels, increasing the risk of heart attack and stroke.
- Kidney disease: High blood sugar can damage the kidneys, leading to kidney failure.
- Nerve damage (neuropathy): High blood sugar can damage nerves, causing numbness, tingling, and pain in the hands and feet.
- Eye damage (retinopathy): High blood sugar can damage the blood vessels in the retina, leading to vision loss.
- Foot problems: High blood sugar can damage nerves and blood vessels in the feet, increasing the risk of foot ulcers and infections.
Living with Type 1 Diabetes
Living with type 1 diabetes requires a lifelong commitment to self-management. However, with proper care and support, people with type 1 diabetes can live full and healthy lives. By working closely with your healthcare team, you can learn to manage your blood sugar levels, prevent complications, and enjoy a good quality of life.
Remember, you’re not alone. There are many resources and support groups available to help you navigate the challenges of living with type 1 diabetes.